Geographical variations in pathways to emergency hospital admissions in infants in England
Selina Nath, Russell Viner, Kate Lewis, Hardelid Pia
UCL Great Ormond Street Institute of Child Health
Background: Accident & Emergency (A&E) attendances and subsequent emergency hospital admissions have been increasing among infants in England over the last decade. The pattern of A&E attendances and emergency admission is not uniform across England. However, it is not clear whether pathways to emergency hospital admissions vary across the country, and to what extent any geographical variations are explained by underlying differences in the population at risk. Our aim was to i) examine variations in pathways to A&E attendances and admissions in infants < 1 years old (a vulnerable age group) by regions and local areas across England; and ii) understand what proportion of these variations could be explained by factors such as gestational age, birthweight and socio-economic status.
Methods: We used data from the English Hospital Episodes Statistics (HES) databases between financial years 2012/13 – 2016/17; A&E dataset for attendances and Admitted Patient Care for emergency admissions (via A&E and direct admissions not via A&E). A&E attendances and emergency admission of infants < 1 years old were extracted and merged with an existing linked HES mother-baby birth cohort, which included variables indicating risk factors such as birth weight, gestational age, maternal age, delivery mode and ethnic group. Children were followed up from the discharge date of their birth admission until their first birthday. Four outcomes were generated relevant to the emergency care pathway; 1) A&E attendance only, 2) emergency admission via A&E attendance, 3) direct emergency admission without attending A&E, and 4) no A&E attendance or emergency admissions. We calculated rates of these outcome events per 1000 child-years with 95% Confidence Intervals (CI) by government office region, local authority and according to socio-economic and clinical risk factors.
Results: The study population included 1,277,962 attendances and 969,637 emergency admissions among 3,100,110 children. The total event rates were 1081/1000 child-years (95%CI: 1080 - 1083) for A&E attendances and 529/1000 child-years (95%CI: 528 - 530) for emergency admissions. Overall, 656,154 (68%) emergency admissions were via A&E and 313,483 (32%) were direct admissions to a ward, with 288,027/313,483 (92%) of direct admissions coming from general practitioners. The proportion of admissions directly to a ward varied from 2% in London to 19% in North West of England. London had the highest rate of A&E attendances (1338/1000 child-years, 95%CI: 1336-1342), but the lowest emergency admission (361/1000 child-years, 95%CI: 359-344). In contrast, the North West of England had the highest emergency admission rates (722/1000 child-years, 95%CI: 720-726) but lower A&E attendances (1227/1000 child-years, 95%CI: 1223-1231) compared to London. Boys, infants born extremely preterm (<28 weeks gestation) and with low birthweight (<2500 grams) had the highest A&E attendances [1161/1000 (95%CI: 1160-1163); 3432/1000 (95%CI: 3372-3494), 1578/1000 (95%CI: 1571-1585) respectively] and emergency admissions (583/1000; 2707/1000, 942/1000 respectively) within the first year of their life.
Implications: There are large variations in A&E attendances and emergency admission across England. A substantial proportion of infants are admitted directly, primarily via general practitioners, and do not attend A&E, particularly outside London. Understanding how care pathways vary across the country and among children with different clinical and socio-economic risk profiles is crucial in order to design interventions to reduce acute secondary care use among infants.
NHS 111 and attendance at hospital after a 111 call – a cross sectional analysis of routine linked urgent and emergency care data
Colin O'Keeffe, Jen Lewis, Richard Jacques, Rebecca Simpson, Tony Stone, Suzanne Mason
University of Sheffield
Background: The NHS 111 telephone advice and triage service was set up to improve access to urgent and emergency care (UEC) for patients in England and direct them to the correct level of care to provide for their health needs. The NHS Long Term Plan is committed to NHS 111 as part of an integrated urgent care approach to reduce pressure on hospital services. 1 A national evaluation using a controlled before and after design demonstrated associations between NHS 111 and increased use of some UEC services. 2 However there is a lack of evidence on the impact of 111 on subsequent use of hospital services, particularly in studies using linked data to follow individual patient episodes. 3 The aim of this analysis was to measure attendance at ED (and subsequent hospital admissions) seven days after an NHS 111 call.
Methods: A cross sectional analysis was carried out using routine adult patient episode data collected from Yorkshire and Humber region. All NHS 111 call data, emergency department (ED) and admitted patient care episode data for the period 2013-2017 was linked. Full HRA ethical approval and additional Section 251 HRA Confidential Advisory Group (CAG) approval was received to process identifiable patient data for linkage, after which the dataset was pseudoanonymised. The primary outcome was the number (%) of patients attending ED within 7 days of the call by 111 disposition and the number (%) subsequently admitted via ED.
Results: There were 3,631,069 NHS 111 calls for the period in patients over 15 years of age. Overall, the number of patients attending ED within 7 days of the 111 call was 839,172 (23.1%). The number of patients admitted (subsequent to the ED attendance) in the period was 322,369 (8.9% of 111 calls and 38.4% of those attending ED).
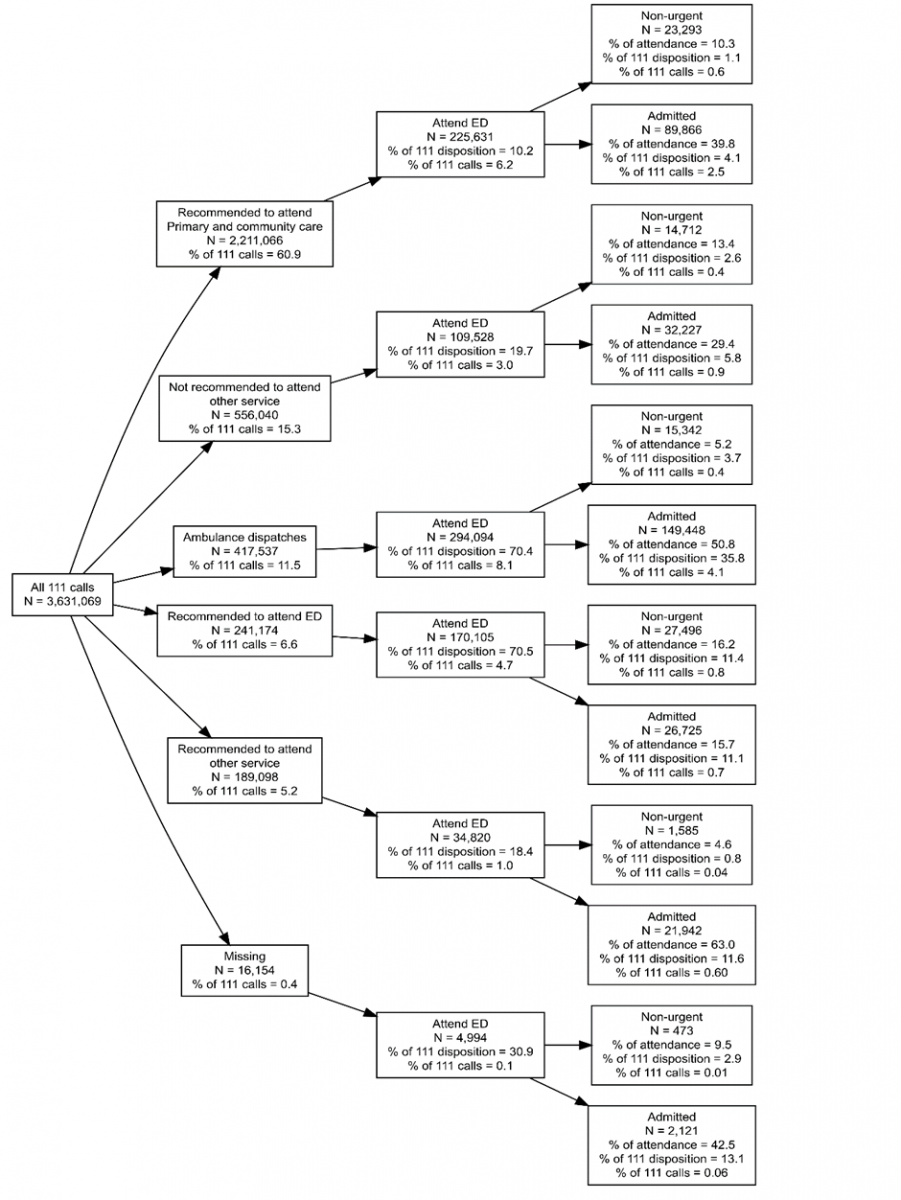
The flow of patients through to hospital by 111 disposition is shown in Figure 1 with the numbers and % of patients attending ED and subsequently admitted to hospital. The number and % of patients who received either a recommendation to attend ED or had disposal ‘ambulance dispatched’ was 658, 711 (18.1%). Of these ‘acute/emergency’ disposals, 464,199 (70.5%) patients attended ED and 176,213 were admitted (37.9% of the ED attendances from this category).
The number (%) of patients receiving a disposal of either ‘primary/community care’, ‘attend other service’ or ‘not recommended to attend another service’ was 2,956,204 (81.4%). The number (%) of these less acute categories of patients who attended ED was 369,979 (12.5%). Overall these less acute disposition categories made up 44.1% of ED attendances in our cohort of NHS111 callers. 144,035 of these less acute categories were admitted (38.9% of these disposal categories that subsequently attended ED).
Conclusion: Large numbers of patients who contact the NHS 111 telephone advice service and who receive a low acuity disposition (e.g primary or community care) are subsequently attending ED. Furthermore, a large proportion of those attending in these categories are subsequently admitted to hospital. The extent to which patients receiving low acuity 111 dispositions have received subsequent advice from another health professional to attend ED, or who choose to attend regardless of advice is not possible to ascertain from our data. Further investigation of these patient pathways is required.
References:
-
NHS England. The NHS long term plan, 2019. https://www.longtermplan.nhs.uk/wp-content/uploads/2019/01/nhs-long-term-plan.pdf
-
Turner J, O’Cathain A, Knowles E, et al. Impact of the urgent care telephone service NHS 111 pilot sites: a controlled before and after study. BMJ Open 2013;3:e003451–e003451. doi:10.1136/bmjopen-2013-003451.
-
Wolters A, Robinson C, Hargreaves D et al. Predictors of emergency department attendance following NHS 111 calls for children and young people: analysis of linked data. https://www.biorxiv.org/content/biorxiv/early/2018/02/06/237750.full.pdf
Figure 1: Flow of patients up to 7 days after NHS 111 call (by 111 disposition advice)
Self-management interventions to reduce healthcare utilisation and improve quality of life among patients with asthma: a systematic review and network meta-analysis
Alex Hodkinson(1), Peter Bower(1), Christos Grigoroglou(1), Salwa Zghebi(1), Hilary Pinnock(2), Evangelos Kontopantelis(1), Maria Panagioti(1)
(1)University of Manchester, (2)University of Edingburgh
Background: Asthma is one of the most common chronic conditions worldwide. Guidelines for treating asthma recommend the use of self-management interventions. However, it is unclear which self-management models are most effective at reducing healthcare utilization and improving quality of life (QoL).
Methods: We performed a systematic review and network meta-analysis (NMA) of randomised controlled trials to compare the effects of three different Self-management intervention models (multi-disciplinary case-management, regularly-supported self-management and minimally-supported self-management) and self-monitoring models, against usual care and education. We searched MEDLINE, the Cochrane library, CINAHL, EconLit, EMBASE, Health Economics Evaluations Database, NHS Economic Evaluation Database, PsycINFO and ClinicalTrials.gov for published and unpublished trials from January 2000 to April 2019. We assessed risk of bias in accordance to the Cochrane Handbook and certainty of evidence using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) framework. The primary outcomes include healthcare utilization (i.e. hospitalisation or emergency visit) and QoL. Summary standardised mean differences (SMDs) and 95% credible intervals (95%CrI) were estimated using Bayesian NMA with random-effects. Heterogeneity was quantified with heterogeneity-variance (τ2) and through inconsistency analysis. Publication bias was assessed with funnel plots. This study is registered with PROSPERO, number CRD42019121350.
Results: From 1,178 citations we included 105 trials comprising 27,767 participants. In terms of healthcare utilization, both multi-disciplinary case-management (SMD=-0.18, 95%CrI: -0.32 to -0.05) and regularly-supported self-management (SMD=-0.30, 95%CrI: -0.46 to -0.15) were significantly better than usual care. For QoL, only regularly-supported self-management (SMD = 0.54, 95% CrI: 0.11 to 0.96) showed a statistically significant increase when compared to usual care. For trials including adolescents/children (aged 5-18 years), only regularly-supported self-management showed statistically significant benefits (healthcare utilization: SMD=-0.21, 95%CrI: -0.40 to -0.03; QoL: SMD=0.23, 95% CrI: 0.03 to 0.48). Multi-disciplinary case-management (SMD=-0.32, 95%CrI: -0.50 to -0.16) and regularly-supported-self-management (SMD=-0.32, 95%CrI: -0.53, -0.11) were most effective at reducing healthcare utilization in patients with symptoms of severe asthma at baseline.
Implications: This is the largest study to use NMA to assess the relative merits of different models of self-management in the treatment of asthma. We conclude that regularly-supported self-management is the most optimal intervention model for improving healthcare utilisation and QoL.
Evaluating a local Clinical Commissioning Group’s pre-surgical health optimisation policy: a feasibility study
Lauren Scott(1), Joanna McLaughlin(2), Lucie Owens(3), Rebecca Reynolds(4), Amanda Owen-Smith(5), Liz Hill1, Russ Jago(5), Sabi Redwood(1), Ruth Kipping(5)
(1)NIHR ARC West, University of Bristol, (2)University of Bristol & Bath and North East Somerset Council, (3)NHS Bath and North East Somerset Clinical Commissioning Group, (4)Bath and North East Somerset Council, (5)University of Bristol
Background: In our local area, the pathway for patients who present to their GP with potential requirements for hip or knee surgery is referral to a team of physiotherapists for approximately six weeks of treatment, followed by a decision about whether or not onward referral for surgery is required.
In late 2017, the local clinical commissioning group (CCG) introduced a health optimisation (HO) policy whereby smokers or those with a body mass index (BMI) ≥30kg/m2 are supported to stop smoking or lose weight for three months prior to treatment, via a ‘healthy lifestyle’ programme. Similar policies are in place in many regions, but the evidence base is lacking. Evaluation is important as it may identify public health benefits or impacts on health inequalities.
Methods: A collaboration between academic and service provision partners developed a study to determine the feasibility of collecting, linking and describing routinely available data on characteristics and progression through the pathway of patients eligible or ineligible for HO. Patients referred between February and July 2018 were followed-up for 12 months.
Results: Data linkage across a number of different service providers was difficult but ultimately successful. During the six-month recruitment period, 502 patients were referred to the elective hip/knee surgery pathway by their GP. Of these, 184 (37%) were referred for health optimisation: 155 (84%) for BMI ≥30kg/m2, 7 (4%) for smoking status, 13 (7%) for both, and 9 (5%) who did not meet either criteria. Only 28% of this group accepted referral to a healthy lifestyle programme (the remainder were still required to undergo the 3-month delay to treatment but chose not to take part in a programme during this time). Data on attendance to healthy lifestyle interventions (such as weightwatchers/ slimming world) were not routinely collected and therefore not available for analysis.
The HO group compared to the non-HO group were similar in age and sex but were more socioeconomically deprived. The HO group also included a larger proportion of knee patients (compared to hip patients) than the non-HO group (73.4% vs. 58.2%). The median change in BMI in the HO group was -0.7 (interquartile range [IQR] -2.5 to 0.0) vs. 0.0 (0.0 to 0.0), and both groups showed a small average improvement in Oxford Hip/Knee Score (1 [IQR -2 to 7] vs. 2 [IQR -1 to 8]). Smoking status at the end of the programme was not routinely collected. Similar numbers of patients in each group were referred onto surgery (57.6% vs. 56.3%), but slightly more dropped out of the pathway and did not attend follow-up physiotherapy appointments in the HO group (7.6% vs. 2.8%). For those admitted for surgery during the follow-up period, average length of hospital stay was equal in the two groups (median 3 days, IQR 2 to 4).
Implications: Evaluation of the HO policy is challenging due to the number of organisations and data sources involved in the patient pathway. This study demonstrates that it is feasible to evaluate the policy, but some important data are not collected routinely. It provides valuable insight into an initial cohort of patients impacted by the policy and necessary considerations for future research to evaluate the impact on health inequalities and outcomes.
InFORM: Improving care for people who Frequently call 999: co-production of guidance through an Observational study using Routine linked data and Mixed methods
Ashra Khanom(1), Helen Snooks(2), Alison Porter(2), Alan Watkins(2), Jason Scott(3), Nigel Rees(4), Robin Petterson(4), Ann John(2), Bridie Evans(2), Adrian Edwards(5), Penny Gripper(2), Bethan Edwards(2), Heather Hughes(2)
(1)Swansea University Medical School, (2)Swansea University, (3)Northumbria University, (4)Welsh Ambulance Service, (5)Cardiff University
Background: People who frequently call the 999 ambulance service present an operational challenge to providers and their needs are inadequately met by current service provision. We aimed to understand patterns and health outcomes of frequent calling and to work with stakeholders to co-produce guidance for formal testing in a future evaluation.
Methods: This mixed methods study will include a scoping review of national and international literature followed by an epidemiological study of callers at the all Wales level exploring health outcomes through anonymised linked data. We will also explore the views of patients using qualitative Bio-photographic interview method with a follow up interview at six months and use focus groups with care providers from across primary and emergency care and the third sector. We will use the Statistical Package for Social Sciences (SPSS) to manage data, and analyse and present quantitative findings and and qualitative data will be analysed thematically.
Results: Findings will include follow up of eligible patients; successful data matching and data linkage; retrieval of outcomes within 6 months. Outcomes will include: adverse events, deaths, emergency admissions; 999 attendances. Qualitative results will include Bio-photographic interviews with completed scrap books and interviews based on the books (n=34). Care provider focus groups (n= 22). Finally we will hold three stakeholder events to co-produce a ‘Guidance for Care’ with stakeholders (patients and care providers).
Implications: High users of the 999-ambulance represent a significant policy challenge to emergency ambulance services and often present with complex needs. This study will inform on the characteristics of callers and how to address their care supported with a co-produced ‘Guidance for Care’ for use by care providers.
What are emergency ambulance services doing to meet the needs of people who call frequently? A national survey of current practice in the United Kingdom
Ashra Khanom(1), Helen Snooks(2), Robert C(3), Adrian Edwards(4), Bethan Mair Edwards(2), Bridie A Evans(2), Theresa Foster(5), Rachael T Fothergill(6), Carol P Gripper(2), Chelsea Hampton(2), Ann John(2), Robin Petterson(7), Alison Porter(2), Andy Rosser(3), Jason Scott(8)
(1)Swansea University Medical School, (2)Swansea University, (3)West Midlands Ambulance Service, (4)Cardiff University, (5)East of England Ambulance Service, (6)London Ambulance Service, (7)Welsh Ambulance Service, (8)Northumbria University
Background: Emergency ambulance services are integral to providing a service for those with unplanned urgent and life-threatening health conditions. However, high use of the service by a small minority of patients is a concern. We aimed to describe: service-wide and local policies or pathways for people classified as Frequent Caller; call volume; and results of any audit or evaluation.
Method: We conducted a national survey of current practice in ambulance services in relation to the management of people who call the emergency ambulance service frequently using a structured questionnaire, for completion by email and telephone interview. We analysed responses using a descriptive and thematic approach.
Results: Twelve of 13 UK ambulance services responded. Most services used nationally agreed definitions for ‘Frequent Caller’, with 600 – 900 people meeting this classification each month. Service-wide policies were in place, with local variations. Models of care varied from within-service care where calls are flagged in the call centre, contact made with callers and their GP with an aim of discouraging further calls; to case management through cross-service, multi-disciplinary team meetings aiming to resolve callers’ needs. No formal audits or evaluations were reported.
Implications: Ambulance services are under pressure to meet challenging response times for high acuity patients. Within – service care focused on reducing calls without addressing patients’ underlying needs, whilst multi-disciplinary case management approaches focused on resolving clinical, social and emotional needs to reduce demand on emergency services. However, there is currently inadequate evidence to inform commissioning, policy or practice development.
What GP practice and CCG factors are associated with emergency hospital admissions for people living with dementia?
Emily Eyles(1), Maria Theresa Redanial(1), Sarah Purdy(2), Kate Tilling(2), Yoav Ben-Shlomo(2)
(1)NIHR ARC West, (2)University of Bristol
Background: As populations age, dementia is a condition of increasing concern Among adults over 65 of age in England, 4.3 people per 100 population have been diagnosed with dementia. They account for two thirds of all hospital admissions in this age group. Dementia costs more than cancer, stroke, or heart disease, at £26 billion per year in the United Kingdom. Many hospital admissions of people with dementia are for diagnoses which could be treated in primary care. . Dementia is one of the leading chronic conditions in terms of variability in ambulatory care sensitive conditions (ACSC) admissions by general practice, even after controlling for demographic factors. Ambulatory care sensitive conditions (ACSCs) are potentially avoidable with respect to hospital admission, if managed appropriately in primary or social care. Unplanned hospital admissions in England make up 67% of hospital bed-days, which costs £12.5 billion per year. This study explores the effect of some general practice (GP) and clinical commissioning group factors on unplanned hospital admissions of people with dementia in England.
Method: We used admission data on people with dementia from the Hospital Episode Statistics (HES) GP practice data on practice size, quality of care, practice rating, and demographics collected from the GP practice profiles and the qualities outcome framework (QOF) , and clinical commissioning group (CCG) programme budgeting benchmark tool data for the percent of the CCG budget allocated to mental health care. We examined the association of organizational characteristics of practices and CCGs with ACSC and non-ACSC admissions. ACSC admissions are those deemed to be preventable if they can be treated in primary care, such as complications of diabetes. An example of a non-ACSC admission would be for ischaemic heart disease. The dataset was divided to look into ACSC and non-ACSC admissions.
We used Bayesian multilevel linear regression models, with the CCG as the second level, and practices as the first level. This type of modelling allows for the effect of the CCGs and GP practice characteristics on hospital admissions to be examined separately. This also allows for the variability between CCGs and GP practices to be examined, including how much of there it is and which level accounts for more. Potential risk factors included were practice demographics (average age of patients at the practice, practice access ratings, practice achievement of quality and outcomes framework (QOF)) the percent of the CCG budget allocated to mental health care, and geographical characteristics of the practice, such as region. The multilevel models were specified using MLWiN, using the runmlwin package in Stata 15.1.
Results: More than 90% of the variability in hospital admissions can be attributed to GP practice level differences for both ACSC and non-ACSC admissions. Increased admission rates were associated with practices located in areas of higher deprivation, whereas rurality and larger practice population were associated with a decrease in admissions. However, the CCG does remain important: the percent of its budget allocated to mental health care reduces ACSC admissions, with the opposite effect found in non-ACSC admissions, indicating that people with dementia in CCGs which spend more on mental health will rightfully be sent to hospital with non-ACSCs.
Implications: Highlighting general practice factors affecting emergency admission from ACSCs could help in the management of PWD at risk in primary and social care settings. This can reduce the number of unplanned hospital admissions, which can help improve all aspects of care. Helping to prevent avoidable admissions for PWD would relieve some of the stress on health services and improve quality of life for people with dementia.
