Shoulder pain surgery: one popular procedure not backed by evidence
Timothy Jones(1), Andrew Carr(2), David Beard(2), Myles-Jay Linton(3), Leila Rooshenas(3), Jenny Donovan(3), William Hollingworth(3)
(1)NIHR ARC West, (2)Nuffield Department of Orthopaedics, Rheumatology and Musculoskeletal Sciences, University of Oxford, (3)University of Bristol
Background: Health and social care services are straining at the seams following increasing demand for services from an ageing population with more complex needs. It is vital that commissioners make evidence-based decisions to maximise the effectiveness of hospital care budgets and benefit the overall health of the population.
NHS England has recently commissioned a consultation regarding the use of 17 hospital procedures, one of which is subacromial decompression surgery for shoulder pain. Shoulder pain is common, with a lifetime prevalence of up to 67%. It is often considered to be caused by a bony ‘spur’ forming on part of the shoulder blade, leading to inflammation in the surrounding tissues. Subacromial decompression removes this bony spur. Several RCTs have compared subacromial decompression to exercise or physiotherapy for relief of shoulder pain or improvement in shoulder function, with little evidence of effectiveness.
In this study we use subacromial decompression for shoulder pain as an example to explore the relationship between evolving evidence and clinical practice for hospital procedures, including how many procedures were performed over the last 10 years and how much money was spent before RCT evidence raised questions about the procedure’s value. We compare procedure rates to other countries, discuss how the NHS might reduce the numbers of these procedures, and how we might reduce ineffective care more generally.
Methods: We used routinely collected hospital data from the Hospital Episode Statistics (HES) Admitted Patient Care (APC) 2007/8-2016/17 and population estimates from the Office for National Statistics. Procedure rates were standardised for age, sex, deprivation, and ethnicity. Healthcare Resource Group codes were linked to Payment by Results tariffs for each year to estimate costs.
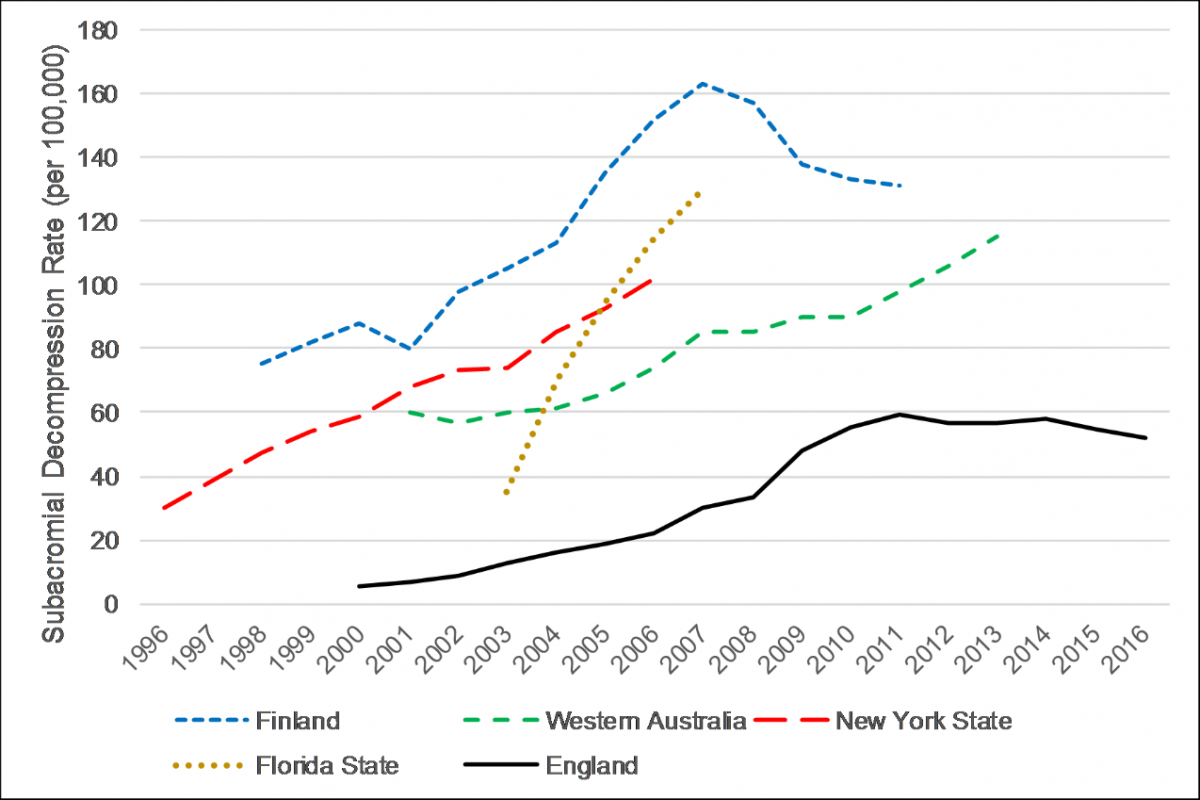
Results: Without robust clinical evidence, the use of subacromial decompression in England increased by 91% from 15,112 procedures (30 per 100,000 population) in 2007/8, to 28,802 procedures (52 per 100,000 population) in 2016/17, costing over £125 million per year. Rates of use of subacromial decompression are even higher internationally: Finland (131 per 100,000 in 2011), Florida State (130 per 100,000 in 2007), Western Australia (115 per 100,000 in 2013), and New York State (102 per 100,000 in 2006). Two randomised placebo-controlled trials with low risk-of-bias, FIMPACT (Paavola et al., 2018) and CSAW (Beard et al., 2018), have recently shown the procedure to be no more effective than placebo surgery (i.e. diagnostic arthroscopy only).
Implications: Without good evidence, nearly 30,000 subacromial decompression procedures have been commissioned each year in England, costing over £1 billion since 2007/8. Even higher rates of procedures are carried out in countries with less regulated health systems. High quality randomised trials need to be initiated before widespread adoption of promising operative procedures to avoid over-treatment and wasted resources. It remains to be seen whether recent RCT findings will be successfully implemented to reduce subacromial decompression rates and save money. We need to research effective methods to prevent or desist the use of ineffective procedures.
Can Hospital Accreditation influence healthcare workforce? Lessons learnt from Accrediting public hospitals in the United Arab of Emirates.
Amna Alshamsi, Louise Thomson, Angeli Santos
University of Nottingham
Abstract: Seeking accreditation has become a popular process in evaluating the quality of healthcare services. Accreditation is an external inspection process, which assesses the performance of healthcare facilities to a defined set of standards, supports the promotion of patients’ health and safety, and improves the quality of healthcare management and leadership. Although extensive research has been carried out to assess the quality of healthcare services and promote patients’ health and safety, very little is currently known about the influence of accreditation on employees’ health and organisational outcomes. Furthermore, burnout, which is characterised by having increased feelings of emotional exhausting and cynical behaviours, is a serious phenomenon in healthcare research demonstrating severe consequences on healthcare professionals, patients and organisations. While healthcare accreditation might be appealing to managers and stakeholders, it is vital to examine the influence of such process and the entailed consequences affecting healthcare professionals.
Aim: This poster aims to evaluate psychosocial risk factors that go hand in hand with the accreditation process in hospitals and their influence on healthcare workers’ psychological health (i.e. Burnout) and organisational safety outcomes (i.e. Work engagement). Furthermore, this poster will outline different factors that influenced workers’ health while preparing for such accreditation.
Methods: A longitudinal within-subject design was employed on five public hospitals. Using self-reported measures. Items on the scales examined the experienced psychosocial factors during the course of accreditation, such as increased job demands and inadequate psychosocial resources. The study targeted hospitals in the United Arab of Emirates based on the accreditation plan for the year of 2019/2020. SPSS software was used to analyse the data using MANOVA repeated measures which assumes that independent variables, such as increased job demands and lack of adequate social resources will have observed effects on workers’ health and work engagement.
Results: This poster will report findings of the study conducted in recent accredited healthcare facilities, which aims to measure the influence of healthcare accreditation on healthcare professionals’ psychological health and organisational outcomes. An initial independent sample T-Test reported a non-significant difference in Burnout experienced by male and female healthcare providers (N=723), t (721) = 0.120, p > 0.05, 95% C.I [-0.424 – 3.670]. Both male and female experience the same level of burnout. Furthermore, work engagement showed a non-significant difference between both genders. In addition, findings will argue that the process of healthcare accreditation could increase the risk of psychosocial risks related to employees’ psychological health and organisational safety outcomes such as patients’ safety.
Implications: The implication for the future organisational support and commitment in reducing psychosocial risks during the accreditation process and the contribution of this study to the felid of Occupational Health and Psychology in developing countries of the Eastern Mediterranean region will be discussed in the poster.
Evaluation of the implementation of Freedom to Speak Up Guardians in NHS England
Aled Jones(1), Jill Maben(2), Carys Banks(2), Daniel Kelly(1), Joanne Blake(1), Russell Mannion(3), Mary Adams(4)
(1)Cardiff University, (2)University of Surrey, (3)University of Birmingham, (4)King's College London
Background: Healthcare staff who raise concerns, or “speak up”, about the quality of patient care make an important contribution to patient safety. However, several reports into serious and avoidable patient care failures strongly suggest that problems of silence (employees not speaking up), deafness (organizations not hearing) and disregard (organizations not acting on concerns) are pervasive internationally. In response to these issues NHS England introduced the “Freedom to Speak Up Guardian” (FTSUG) role in 2016. Three interlinked objectives for the FTSUG role are to: (a) create an environment where speaking up is part of the normal routine business of NHS organisations (b) promote culture change to prevent employees being victimised for speaking up and (c) ensure NHS organisations learn from employees who speak up. This is the first in-depth study of the implementation of this internationally novel and important role.
Methods:
Research questions
-
How are FTSUGs being variously deployed, managed and held accountable for their work?
-
How is the work of FTSUGs defined and negotiated in relation to the work of others who also deals with employee concerns and patient safety at local and national levels?
-
Do different models for implementing the FTSUG role impact on the ‘freedom to speak up’, both in the ways that employees raise concerns and how these concerns are responded to?
Data collection
consisted of three interlinked work packages (WP)
WP1: systematic evidence synthesis of international literature of ‘Speak Up’ strategies and interventions undertaken in healthcare.
WP2: 87 telephone interviews with FTSUGs.
WP3: six qualitative case studies examined implementation of FTSUG roles via semi structured interviews with FTSUGs, organisational stakeholders and those speaking up via the FTSUG (n=100). In addition, observational data were collected via shadowing the FTSUG, attendance at meetings (e.g. board meetings, team meetings), walkrounds and training events (induction, team training).
Data analysis:
descriptive statistics of WP2 data and thematic analysis of qualitative data generated in WP2 & WP3.
Selected results:
Time allocated to the role: The majority of FTSUGs interviewed were allocated two days or less to undertake the role. Only 11 of the FTSUGs interviewed were implemented full-time. Unsurprisingly, one of the most significant challenges identified by interviewees was the lack of time availability for the role, which often necessitated undertaking some of the role in their own time.
Dual role: Most FTSUGs were appointed to undertake the role alongside pre-existing roles within the organisation, ranging from directors of nursing, head of employee relations to speech and language therapists, radiographers, patient safety managers and chaplains. When shared with another role, the FTSUG role was allocated less hours (or no hours. Having dual roles both enhanced and restricted the Guardian role.
Wellbeing & support: The responsibilities associated with speaking up weigh heavily on FTSUGs’ shoulders. Most FTSUGs reported feeling supported by the organisation. Some received practical support to cope with the stressful demands of the role, such as clinical supervision or counselling therapy. Others had no-one to “offload” to. FTSUGs reported experiencing sleeplessness, migraines and mental exhaustion as a result of undertaking the role.
Role discontent: The majority of the concerns raised did not relate directly to patient safety, but to time-consuming cases of staff bullying. Many interviewees expressed discontent with the guidance/support available and how bullying concerns were disproportionately and ‘incorrectly’ occupying their time and affecting their own well-being.
Implications: Minimal policy guidance on the implementation of the FTSUG role has resulted in large variation in the resourcing and deployment of the role. Most organisations chose to invest relatively little resource, resulting in FTSUGs struggling to oversee several complex and contentious concerns, often whilst working alone and/or undertaking other substantive organisational roles.
Developing and sharing learning about improving patient flow and patient and staff experiences through a health care system: Evaluating the Flow Coaching Academy Programme
Amanda Watt(1), Miriam Broeks(2), Tom Ling(2)
(1)The Health Foundation, (2)RAND Europe
Background: The Flow Coaching Academy (FCA) programme aims to empower frontline health and care staff to improve patient flow and patient and staff experience through a health care system, and develop a learning network of Flow Coaching Academies across the UK. The programme was launched in 2015 and is funded by the Health Foundation. A team at Sheffield Teaching Hospitals NHS Foundation Trust (STH) developed a curriculum to build team coaching skills and improvement science knowledge of frontline health and care staff working at care pathway level.
The STH hosts and delivers the FCA programme, working with a number of NHS Trusts to deliver the intervention across the UK. The ambition of the programme is to embed the FCA approach around the UK and transform the approach to improving flow across condition pathways. Since the programme was established, seven local Flow Coaching Academies at NHS trusts have been set up, with up to three more to be set up in 2020.
Method: Between 2016 and 2019 the Health Foundation commissioned RAND Europe to conduct an independent evaluation of the FCA programme. The evaluation was principally formative and provided feedback to support the continuous improvement in the design and delivery of the programme. The evaluation used mixed methods and explored the effectiveness of the FCA programme in training coaches, assessed the impact of the programme within pathways, including the ability of the coaches to develop local capability and capacity, and contribute to improvements in patient flow in different contexts, and evaluated early spread beyond initial sites.
Results: The evaluation found promising evidence showing that the distinctive FCA approach leads to improvements in technical and personal skills of staff (e.g. improved confidence, better working relationships, reduced hierarchies, etc.), as well as in selected pathways. It identified the challenges experienced by healthcare staff in collecting and analysing data to quantify both ‘human’ and ‘technical’ impacts of the programme. The evaluation also identified the areas where further knowledge is needed for the local FCAs to continue having impact and for the programme to continue expanding its learning network of FCAs. It also identified the importance of considering patient experience to provide tailored improvement and it notes the wider implications of the findings on ensuring impact of QI approaches more widely.
This presentation will reflect on currently available evidence on the Flow coaching improvement approach, and discuss lessons learned from the evaluation and identified challenges (1) specific to Flow coaching and (2) applicable more widely to other QI approaches.
Implications: The FCA programme is a promising approach to QI that was designed to be tailored to context. Dixon-Woods and Martin (2016) have cautioned that “too many QI interventions are seen as ‘magic bullets’ that will produce improvement in any situation, regardless of context. Moreover, too much improvement work is undertaken in isolation of the local level, failing to pool resources and develop collective solutions”. Whilst multiple factors can underlie this issue, this highlights the importance of developing and using a QI approach following careful consideration of the context in which it will operate, something the FCA programme does. It seeks to pool resources and develop collectively agreed solutions, and it is sensitive to unintended harmful consequences. These characteristics mark it out as a valuable addition to available QI approaches.
Learning for the FCA continues. To understand the overall impact of the programme, the Health Foundation commissioned a summative evaluation in early 2020. This evaluation seeks to develop learning about FCA improvement to those participating in the programme and provide system-wide knowledge about how to scale, embed quality improvement across multiple sites, clinical pathways, and settings.
Exposure to the views and behaviours of other health professionals: a systematic review and meta-analysis of social norms and clinical behaviour change
Sarah Cotterill(1), Mei Yee Tang(1), Rachael Powell(1), Jane Roberts(2), Laura McGowan(1), Elizabeth Howarth(1), Benjamin Brown(1), Sarah Rhodes(1)
(1)University of Manchester, (2)Northern Care Alliance
Background: Health professionals routinely conduct behaviours which impact on patient care, but may face challenges in adopting behaviours which follow best practice. Some strategies to change professionals’ behaviour make use of social norms, and can be delivered as part of audit and feedback. We define a social norm intervention as one which seeks to change the clinical behaviour of a target health professional by exposing them to the values, beliefs, attitudes or behaviours of a reference group or person. This study summarised evidence on (i) the effect of social norm interventions on health professional behaviour’ (ii) the contexts, modes of delivery and behaviour change techniques (BCTs) associated with effectiveness.
Methods: A systematic review and meta-analysis of randomised controlled trials was conducted. Searches were undertaken in seven databases. Full text screening, data extraction, assessment of bias and coding of BCTs were undertaken independently by two reviewers. The primary outcome was compliance with a desired health professional behaviour and the secondary outcome was patient health. Outcomes were converted into a standardised mean difference (SMD). To assess the effect of social norms on the behaviour of health professionals we performed meta-analyses on the combined estimates from individual studies and presented forest plots, stratified by five social norm BCTs (social comparison, credible source, social reward, social incentive and information about others’ approval). Sources of variation in social norm BCT, context and mode of delivery were explored using forest plots, meta-regression and network meta-analysis.
Results: The review found 106 unique trials. Interventions that included social norms were associated with an improvement in health professional behaviour (primary) of 0.08 SMD (95% CI 0.07 to 0.10) (n=100), and in patient outcomes of 0.17 SMD (95% CI 0.14 to 0.20) (n=14), on average. Heterogeneity was high (I2 85.4%). Social comparison (n=81) and credible source (n=7) were each, on average, effective in changing behaviour, both separately and when combined together (n=8). Social comparison was most effective when combined with social reward (n=2) or prompts and cues (n=5). Social reward on its own seemed unlikely to be effective, but the number of studies was small (n=2). These results were consistent across meta-analysis, meta-regression and network meta-analysis.
Social norms interventions appeared to be effective across a wide range of NHS contexts: with doctors (n=68) other health professionals (n=12), in primary (n=56) and secondary (n=27) care, but not with nurses or allied health professionals (n=5) or in community and care settings (n=8). Social norms were effective, on average, when targeting a wide range of behaviours including prescribing (n=40), test ordering (n=21), and management of health conditions (n=23). Formats including email, written, web and mixed were all effective, but face-to face delivery was not effective, on average. Delivery once was, on average, more effective than multiple times (SMD 0.25 v 0.06). Results may be affected by small numbers in some categories and confounding.
Implications: Social norms interventions have been frequently used by healthcare organisations as a way of improving how health care is delivered. This review suggests that the overall result is modest and very variable, but there is the potential for social norms interventions to be applied at scale, and when optimally designed, they can have a positive effect on the target behaviour and resulting patient outcomes. The most effective social norms interventions appeared to be providing approval of the desired behaviour from a credible source, and social comparison with peers combined with social reward or prompts and cues. These interventions can be effective in a variety of NHS contexts and across different modes of delivery. In contrast to other research, we found no evidence that delivery more than once is necessary.
Insights on the impact of accreditation on healthcare workers
Amna Alshamsi, Louise Thomson, Angeli Santos
University of Nottingham
Background: Although the impact and outcome of healthcare accreditation remain debatable, the growth of such program has increased significantly and many countries mandate accreditation to improve the service delivered to patients. Recent studies have noticed observed consequences to this inspection process, such as increased workload and elevated stress level. Accreditations assess the performance of healthcare facilities to a defined set of standards supporting the continuous quality improvement concept. Although extensive research has been carried out to assess the quality of healthcare services and promote patients’ health and safety, very little is currently known about the influence of accreditation on employees’ health and organisational outcomes. While healthcare accreditation might be appealing to managers and stakeholders, it is vital to examine the influence of such process and the entailed consequences affecting the psychosocial safety climate (PSC), which reflects policies, practices, and procedures that protect workers’ psychological health. Previous research on the PSC was found to be positively linked with job resources and negatively associated with job demand. Therefore, this study aims to observe different factors, which played a role in influencing workers’ health while preparing for such accreditation.
Aims: This presentation will share finding from recent studies, which explored and tested the extension of the Psychosocial Safety Climate (PSC) to the Job Demand-Resource (JD-R) model, in a range of hospitals at different stages of their accreditation status. In addition, the presentation will highlight observed different factors playing a role in influencing workers’ health while preparing for such accreditation.
Methods: A mixed method study design was conducted using semi-structured interviews and longitudinal surveys to explore and examine changes induced by the accreditation process. Twenty-seven semi-structured interviews and four focus group discussions were delivered followed by online surveys during the course of accreditation. Online surveys measured job demands, job resources, psychosocial safety climate, burnout, and work engagement. The study took place in public hospitals (N = 8) in the United Arab of Emirates (UAE). Data were analysed using NVivo and SPSS software.
Results: Interviews have shown a prevalent number of psychosocial risks during the course of accreditation. Healthcare providers (HCP) faced increased work demands during such process as work demands were perceived to influence their health, family, and patients’ care. On the other hand, teamwork and co-worker support were vital to ease the effect of such demands. In addition, Initial analysis found a strong positive correlation between burnout level among HCPs and job demands three months before accreditation, r (723) = .66, p < .001. Furthermore, reduced patients’ care was highly correlated with job demands, r (726) = .62, p < .001 three months before the inspectors visit.
This presentation will report final results of the study conducted in recent accredited healthcare facilities in the United Arab of Emirates. Findings will argue that increased job demands and decreased PSC during the process of healthcare accreditation could increase psychosocial risks related to employees’ psychological health and organisational safety outcomes such as patients’ care.
Implications: The implication for the future organisational support and commitment in reducing psychosocial risks during quality inspection programs and the contribution of this study to the felid of Occupational Health and Psychology in healthcare services.
