The Cost of Community Research
Caroline Brundle (1), Nicola Harrison (1), Anne Heaven (1), Andrew Clegg (2)
(1) Bradford Teaching Hospitals NHS Foundation Trust, (2) University of Leeds, Bradford Teaching Hospitals NHS Foundation Trust
Background: A key policy focus for the 2019 NHS Long Term Plan (https://www.longtermplan.nhs.uk/) is for health services to be delivered to people in their communities. To support a robust evidence base for the organisation and delivery of services, clinical trials will need to be designed to account for community-based recruitment. However, there is currently limited information around the time and cost of recruiting participants in the community, meaning that development of research applications and completion of cost attribution documentation, for example the Schedule of Events Cost Attribution Template (SoECAT), is problematic.
Aim: To establish the amount of researcher time it takes to consent community-dwelling older people to the Personalised Care Planning for Older People with Frailty (PROSPER) feasibility primary care cluster randomised controlled trial (@ProsperTrial).
Method: After individuals had received study information from their general practice and expressed interest in taking part, home visits were arranged by researchers in order to gain consent and undertake baseline data collection. Two researchers collected timing data during every third visit undertaken over a two-month period (September-October 2019).
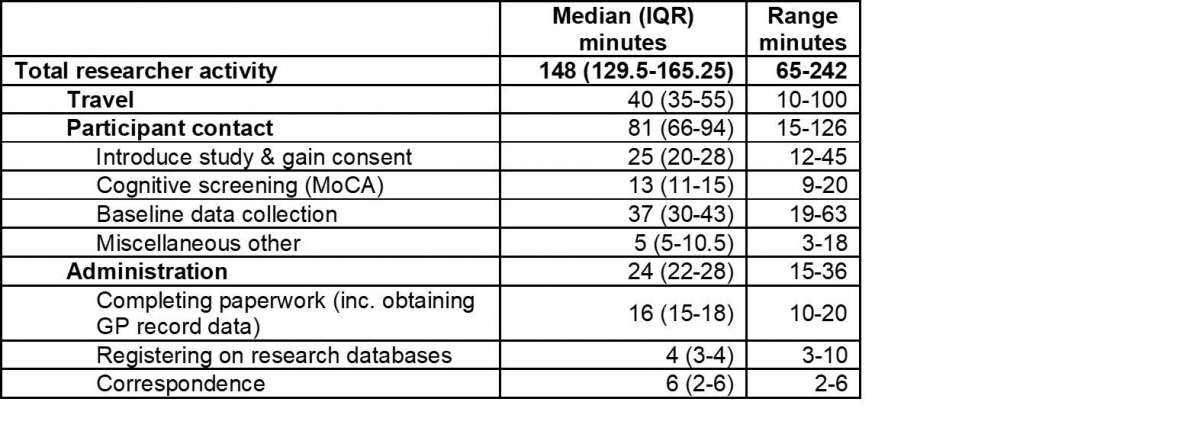
The time taken for travel, visits and administration was recorded on a pro-forma. Visit time was broken down into eight categories including: informed consent; undertaking screening with the Montreal Cognitive Assessment (MoCA); baseline data collection; consultee declaration; carer consent and data collection; and miscellaneous time such as chatting and making tea.
Administration time was broken down into six categories including: completing paperwork and registering patients onto the trial.
Not all sections required completion at each visit depending on issues such as mental capacity and whether a patient had a carer as defined by the study.
Results: Data was collected from 33 visits. 29 individuals visited were recruited to the trial, four declined participation.
The median activity time per visit was 148 minutes. This comprised medians of 40 minutes of travel, 81 minutes of participant contact and 24 minutes of administrative tasks. Further breakdowns of timings are shown below.
Fiddling while Rome Burns? Conducting research with healthcare staff when the NHS is in crisis
Laura Sheard
University of York
Background: The NHS in the UK is said to be crisis, with many areas of the health service struggling to meet increasing demand with fewer resources. The deepening of this crisis over the past few years has led to a lack of healthcare staff on the ground, with increased pressure on those who remain in clinical practice. Consequently, health research is becoming increasingly difficult to conduct. This is having a demonstrable impact on the conduct and findings of, in particular, applied health services research. This presentation will use the Great Fire of Rome as an allegory to understand the above situation.
Methods: I draw on a corpus of data from both my own and other research teams’ experiences of conducting research with healthcare staff over the past five years. This predominantly takes the form of evidence from the published outputs of eight different applied studies but also involves the use of tacit and experiential knowledge gained through fieldwork in an acute hospital setting.
Results: Recruitment and engagement issues across different research studies and clinical environments are often ascribed as being related to individual contexts or settings. Rather, I propose that this is mostly not the case and that these problems are actually writ large across nearly the entire NHS in what could be termed “a context of crisis”. I offer macro and micro level ideas for what can be done to alleviate the worst of this situation – a change in culture and ways of working alongside the need for researchers to employ more pragmatic, rapid methods to engage exceptionally busy healthcare staff.
Implications: This presentation offers a provocative viewpoint that instead of seeking to individualise recruitment and engagement issues in relation to the local context, the research community should publicly acknowledge the universality of this problem in order to bring about meaningful change.
Medical consumerism and the modern patient: a three generational model of challenge, niche market and managed conumerism
Stephen Iliffe (1), Jill Manthorpe (2)
(1) University College London, (2) Kings College London
Background: Many doctors find medical consumerism difficult to work with, preferring ‘patient-centred’ work styles (based on evidence and protocols) to more relational ‘person-centred’ working. Medical consumerism originated as challenges to physician authority, but through its encounters with health services has evolved in different directions.
Methods: We propose a basic model of medical consumerism that includes three generations representing challenges to physician authority, niche market customers and managed consumerism, respectively. All three generations can co-exist and may interact.
Results: The first generation (challenge) is a relatively weak stimulant to competition in the provision of medical care but can promote a rich civil society as well as generate intense conflicts between patients and doctors. We illustrate the first generation with the case of Charlie Gaard. The second generation (customers) enriches niche markets but also creates stressful ethical dilemmas. We illustrate this with the current controversy over textured breast implants. The third generation patient can generally have what s/he wants, but only if s/he is a serious advocate for and practitioner of healthiness. This type of managed consumerism has the potential to foster patients’ full engagement with the NHS, as urged by Wanless in 2002, and we illustrate it with analyses of ‘successful ageing’, ‘self-management’ and ‘prosumerism’.
Implications: This paper begins to explore the implications for research, policy and practice of these generations, and suggests some questions about the different forms of consumerism that medical and other healthcare practitioners might consider.
Learning from a feasibility trial of a simple intervention: Is research a barrier to service delivery, or is service delivery a barrier to research?
Julia Frost, Nicky Britten
University of Exeter
Background: Applied health services research relies upon coordination across multiple organizational boundaries. Our aim was to understand how competing organizational and professional goals enhance or impede the conduct of high quality applied health services research.
Methods: A qualitative study was conducted in two local health care systems in the UK, linked to a feasibility trial of a clinic based intervention in secondary care. Data collection involved 24 semi-structured interviews with research managers, clinical research staff, health professionals and patients.
Results: This study required a dynamic network of interactions between heterogeneous health and social care stakeholders each characterized by differing ways of organizing activities which constitute their core functions; cultures of collaboration and interaction and understanding of what research involves and how it contributes to patient care. These interrelated factors compounded the occupational and organizational boundaries that hindered communication and coordination.
Implications: Despite the strategic development of multiple organizations to foster inter-professional collaboration, the competing goals of research and clinical practice can impede the conduct of high quality AHSR. Attention to the sociocultural boundaries that obstruct communication and coordination can help to ameliorate the tensions between clinical practice and research.
Primary care networks in the English NHS: (another) triumph of hope over experience?
Judith Smith (1), Amelia Harshfield (2), Manbinder Sidhu (3), Sarah Parkinson (2), Natasha Elmore (2)
(1) Health Services Management Centre, University of Birmingham, (2) RAND Europe, (3) University of Birmingham
Background: In July 2019, 1259 primary care networks (PCNs) were introduced across England as part of the NHS Long Term Plan1 to manage a major investment in primary care and general practice. These networks comprise groups of general practices covering a population typically between 20,000 and 50,000 registered patients. New funding is being made available to PCNs via a contract held across practices in the network to develop shared services such as social prescribing, practice-based community pharmacy support, enhanced health services for care homes, digital forms of access to general practice, and more effective early cancer diagnosis.
The Birmingham, RAND and Cambridge (BRACE) Rapid Evaluation Centre, funded by the National Institute of Health Research (NIHR), is undertaking an evaluation of the early implementation of PCNs, investigating what can be learnt from prior research evidence, and examining what is helping and hindering this type of working. The research has a particular focus on the experience of rural as well as urban collaborations, and those places where historically, collaborative working in primary care has struggled to become established.
Method: An initial rapid evidence review was undertaken and reported2, and the results tested out in a workshop of policy makers and practitioners. This helped refine research questions for the empirical stage of the evaluation - case study research in four PCN areas (two rural, one semi-rural and one urban) where methods used include documentary analysis, observation of PCN board and clinical leaders' meetings, semi-structured interviews, and an on-line survey of GPs and practice managers. The results will be analysed and published in an NIHR Journals Library report during summer 2020.
Results: Themes from the rapid evidence review included: the importance of having effective management support and funding; the inevitable variation in progress that will be seen across PCNs, which will likely frustrate policy makers and performance managers and lead to calls for mergers and more ‘pace’; the need for clarity of scope and objectives for PCNs, to avoid them over-promising and under-delivering; and the vital importance of relationships and culture within PCNs and across health economies, which will require sophisticated leadership and management, and extensive support for PCNs.
In this presentation, we will extend and deepen this early analysis by setting out the main findings of our empirical work, and we anticipate that these will include:
- An account of the early experience of PCNs, and what is enabling and hindering their progress
- An assessment of the extent to which this experience differs from, or is similar to, that of prior GP collaborations in the UK and overseas
- The specific issues faced by PCNs in rural areas
- The relationship between pre-existing ‘at scale’ primary care organisations (e.g. super-partnerships, GP federations) and PCNs
- A proposal as to how PCNs might be tracked longer term beyond our rapid evaluation study
Implications: This research provides some of the earliest empirical insights into the implementation of this new policy initiative in the NHS in England, one that is distinctive in using a new contract across collectives of GP practices, with the intention of steering them to focus on specific (and arguably very challenging) population health and service priorities from the NHS Long-Term Plan.
We are employing rapid evaluation methods in a complex and contested policy and organisational context, and will conclude with a reflection on our experience of and learning about using such an approach.
- NHS England (2019) The NHS Long Term Plan. London, NHS England
- Smith J and Harshfield A (2019) Primary Care Networks: a marathon not a sprint. London, Health Service Journal, September 2019
News coverage related to service delivery and organisation of the National Health Service (NHS) in British online newspapers
Katherine Lovejoy, Saprina Moor, Yen-Fu Chen
University of Warwick
Background: The popularity of online news outlets continues to rise with the advance in mobile technologies, which allow easy access to the internet. News articles related to the NHS are frequently featured in online newspapers. Their content and style of reporting could affect the public’s understanding of the NHS and influence people’s opinion and attitude towards it. This study aims to describe main features of news articles published in major British online newspapers related to service delivery and organisation of the NHS, to analyse sources of information quoted in the articles, and to explore whether these are associated with the type and political stance of the newspapers.
Methods: Five major British online newspapers covering different political stances were chosen. These include three broadsheets (defined in a traditional sense rather than by current publication format): The Guardian, The Telegraph and The Times; and two tabloids: The Daily Mail and The Daily Mirror. The Guardian and The Daily Mirror were classified as left-wing while the other three newspapers were classified as right-wing based on a YouGov survey (Smith 2017). Articles published in January, April, July and October of 2019 were sampled from the website of each newspaper either randomly or from the beginning of the chosen months (for newspapers with designated section for health/NHS) until a maximum of 10 articles per newspaper per month was reached. Eligible articles had to be concerned with a topic related to service delivery and organisation of the NHS. Included articles were categorised according to the tier of service (primary or secondary care, or both), topic area (workforce, delays and waiting time, funding, quality and safety, and access to care; multiple categories were allowed), article outlook (negative, neutral or positive) and sources of information quoted. Coding was undertaken independently by two authors and disagreements were arbitrated by the third author. Descriptive statistics were computed for each type of newspapers and political stances, and associations were explored using Chi-squared tests.
Results: A total of 271 news articles were selected and analysed. The Daily Mail contributed to the largest number of articles (73, 27%) while The Guardian contributed to the least (45, 17%). Different topic areas were well covered, with more than a third of the articles reporting on issues related to quality and safety, and access to care respectively. Forty percent of the articles focused on primary care, 44% on secondary care and the remaining covered both. Most articles (223, 82%) had a negative outlook, which appeared to differ between newspaper type (tabloid 87% [n=119] vs broadsheet 78% [n=152], p= 0.051) and political stances (left-wing 88% [n=91] vs right-wing 79% [n=180], p=0.085). Information or comments were obtained from NHS personnel (50% of all articles), government officials (49%), grey literature or routine statistics (38%), charitable organisations (31%), professional societies (30%), patients and carers (19%), published research (13%) and academics (10%). Tabloids were more likely to use information from individual patients/carers than broadsheets (29% vs 11%, p<0.001), whereas right-wing newspapers quoted grey literature and routine statistics more frequently than left-wing papers (43% vs 28%, p=0.011).
Implications: The majority of news articles related to the NHS had negative outlook. This may reflect the tendency for the media to focus on ‘newsworthy’ events, which tend to be negative, but also highlights potential roles of mass media in voicing public concerns and influencing public opinions. The potential impact of the predominantly negative portrayal of the NHS and the observed differences in information sources used between newspapers of different types and political stances may warrant further investigation.
Reference:
Smith M (2017) How left or right-wing are the UK’s newspapers? YouGov [online] Available at: https://yougov.co.uk/topics/politics/articles-reports/2017/03/07/how-left-or-right-wing-are-uks-newspapers
Is health research undertaken where the burden of disease is greatest? Observational study of geographical inequalities in recruitment to research in England 2013-2018
Peter Bower (1), Christos Grigoroglou (1), Laura Anselmi (1), Evangelos Kontopantelis (1), Matt Sutton (1), Mark Ashworth (2), Phil Evans (3), Stephen Lock (4), Steven Smye (4), Kathryn Abel (1)
(1) University of Manchester, (2) KCL, (3) University of Exeter, (4) NIHR CRN
Background: Research is fundamental to high quality care, but concerns have been raised about whether health research is conducted in the populations most affected by high disease prevalence.
Geographical distribution of research activity is important for many reasons. Recruitment is a major barrier to research delivery, and undertaking recruitment in areas of high prevalence could be more efficient. Regional variability exists in risk factors and outcomes, so research done in healthier populations may not generalise. Much applied health research evaluates interventions, and their impact may vary by context (including geography). Finally, fairness dictates that publically-funded research should be accessible to all, so that benefits of participating can be fairly distributed.
We explored whether recruitment of patients to health research is aligned with disease prevalence in England.
Methods:We measured disease prevalence using the Quality and Outcomes Framework in England (total long-term conditions, mental health and diabetes). We measured research activity using data from the NIHR Clinical Research Network, exploring all research, specific clinical specialities, and health services research.
We presented descriptive data on geographical variation in recruitment rates. We explored associations between the recruitment rate and disease prevalence rate. We calculated the share of patient recruitment that would need to be redistributed to align recruitment with prevalence. We assessed whether associations between recruitment rate and disease prevalence varied between conditions, and over time.
Results: There was significant geographical variation in recruitment rates. When areas were ranked by disease prevalence, recruitment was not aligned with prevalence, with disproportionately low recruitment in areas with higher prevalence of total long-term and mental health conditions.
At the level of 15 local networks, analyses suggested that around 12% of current recruitment activity would need to be redistributed to align with disease prevalence. Overall alignment showed little change over time, but there was variation in the trends over time in individual specialties.
When the distribution of health services research was explored compared to total prevalence of long-term conditions, the overall alignment was not markedly different from that for clinical research (approximately 15% of research would need to be redistributed at the level of the 15 local networks).
Conclusions: Geographical variations in recruitment do not reflect the suitability of the population for research.
Health services research does not seem to markedly differ from clinical research on these measures of alignment. This might be contrary to expectation, given the contextual nature of much health services research. The results may be influenced by the fact that a significant proportion of health services research may not enter the CRN portfolio.
Indicators should be developed to assess the fit between research and need, and to allow assessment of interventions among funders, researchers and patients to encourage closer alignment between research activity and burden.
